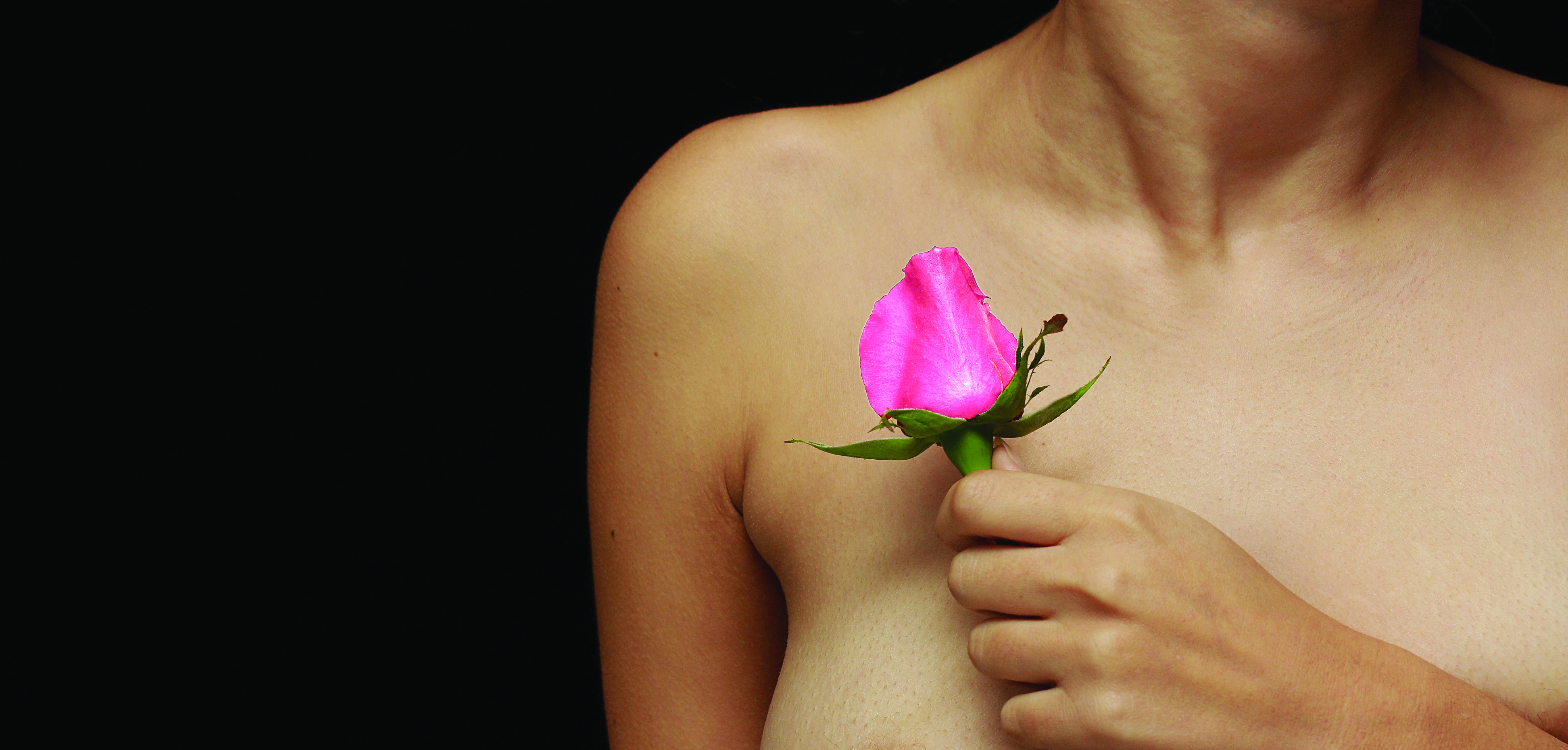
Laura Lisicki has had many titles. Daughter, wife, mother, nurse, nurse practitioner and friend. The one title she never thought she would carry is Breast Cancer Survivor. As a nurse in the Critical Care Intensive Care Unit and then a Nurse Practitioner in family and internal medicine for 23 years, with a focus on women’s health, Laura knows all the risk factors. She knows all the statistics, and she knows what do to if and when something turns up. But all of the knowledge in the world didn’t prepare her for when the provider became the patient.
At 44 years old, Laura found a mass in her breast during a self-exam, the very thing she tells all of her patients to do monthly. But this was different. This wasn’t a patient. This wasn’t Laura, Nurse Practitioner, that found a mass on a patient. This was Laura Lisicki, wife to John and mother of four. This wasn’t supposed to happen to her, “I had no family history and none of the risk factors,” she said. When asked what she did next, she very candidly said, “I went into denial.”
Once the shock of the situation wore off, Laura did exactly what she would have told one of her patients to do, she had a mammogram. They found that she had a five-centimeter tumor that could be seen through her skin, and it was getting larger. They not only found the large tumor on one side, but also precancerous calcifications on the other. After referring with the radiologist and an oncologist, it was determined that for her to have the most successful prognosis she would need to have a double mastectomy. At that point, Laura allowed herself to be the patient, and not the provider. “I picked my team of doctors and I let them help me make the decisions. They decided the course of treatment I should take. I had to let go of that for my own good.” Because of the nature of the tumor that she had, Laura did not have to undergo radiation or chemotherapy. This by no means meant a smooth recovery.
She had a husband, two teenagers and two elementary school children at home and a career. She had to rely on her support network to make it through each day. “My husband was my biggest support and he still is. He went to every single appointment with me. He drained the ports I had, slept at the hospital and never left my side,” she said of her husband of 32 years. It was important to both Laura and John that their children go on with their days with their same routine. This was made possible with the help of friends, family and neighbors. “They cooked for not only me and John, but for the entire house, no matter who was there! We never had an empty fridge!” Even though Laura and John made every effort for their children to go on as “normal” as possible, it still affected them and continues to affect them. “They worried, and still worry. They worry about what could have happen and what might happen,” she said. The unpredictability of cancer means you can never fully prepare. The best you can do is educate yourself and be proactive in your own health.
Laura is now eight years cancer-free and is continuing her medical career as a nurse practitioner educating and caring for women who are in the same place she was eight years ago. As a cancer survivor, she is in a unique position as a medical provider. Unlike most in her field, she has first-hand experience and intimate knowledge of what her patients are experiencing. She embraces the fact that her story can help her to help her patients in a way nobody else can. “You can’t believe how many women in my practice, who together we have found breast cancer that I’ve helped through it, and I think maybe that is why I went through it myself,” she said. Laura’s goal is not only for herself, but for others. “My goal in life as a survivor is to not only make it past 10 years, but to be cancer free for life and to help those around me to be cancer free as well! I am blessed to see the dawn of every day and the faces of those around me that I love, and that is my miracle.”
Statistics and Risk Factors
Like Laura, most people never believe that cancer will directly affect them. Nobody thinks they will become one of the statistics, until they are. Here are some sobering facts about breast cancer from the National Breast Cancer Foundation:
One in eight women in the United States will be
diagnosed with breast cancer in her lifetime
Breast cancer is the most commonly diagnosed
cancer in women
Breast cancer is the second leading cause of cancer
death among women
Although rare in men, an estimated 2,600 men will
be diagnosed each year
Over 2.8 million breast cancer survivors are alive
in the United States today
Unfortunately, in the fight against breast cancer, there is no one risk factor that, if eliminated, will erase a person’s risk of developing the disease. According to the American Cancer Society the main risk factors are things “you cannot change” including:
Being a woman (although, men can have breast cancer)
Getting older
Having certain gene changes
Having a family history of breast cancer; although 8
out of 10 women who get breast cancer do not have
a family history of the disease
Having a personal history of breast cancer
Race and ethnicity
Having dense breast tissue
Early menstruation (before age 12)
Menopause after age 55
There are also several lifestyle-related risk factors associated with breast cancer, including:
Drinking alcohol (2-5 drinks daily increases risk 1 ½ times those who don’t drink alcohol)
Being overweight or obese
Lack of physical activity
Hormone therapy (HRT) after menopause
Laura’s personal experience and professional training are the perfect combination for educating her patients on prevention and detection. The number one piece of advice that she gives her patients is to be aware of your body and any changes you may notice. When treating patients, Laura’s protocol is to always “encourage annual mammograms, self-breast exams monthly and breast exams once per year by a provider.” The best way to be proactive is with monthly self-exams. All women should be familiar with the way their breasts feel and look and should see a medical professional at the first sign of anything different. According to the American Cancer Society, early detection and treatment “are the most important strategies to prevent deaths from breast cancer.” Detection at its earliest stages can promote prompt treatment to slow down or even halt progression.
According to the National Cancer Institute, there are three main tests used by health care providers to screen for breast cancer:
Mammogram
Clinical breast exam (CBE)
MRI in women with high risk of breast cancer
Of these three screening options, mammography is the most common. A mammogram is an x-ray of the breast which may find tumors that are too small to feel. Mammograms are also used to detect ductal carcinoma in situ (DCIS). In DCIS, there are “abnormal cells in the lining of a breast duct, which may become invasive cancer in some women,” according to the National Cancer Institute.
There has been some controversy in recent years as to the appropriate guidelines for when and how often women should have a mammogram. There are some organizations that believe that women age 50 and older should receive a mammogram once per year. The previous thought was to begin annual mammograms at age 40 for those with average risk factors. While the decision on when to begin getting annual mammograms is ultimately up to the patient, the American Cancer Society suggests that women between the ages of “40 and 44 should have the option to start screening with a mammogram every year.” There is agreement across the board, however, that women with elevated risk factors should have a mammogram at the earliest possible time.
One thing to keep in mind when deciding when is the best time to begin annual screening is mortality rates. According to the Susan G. Komen organization, “From 1989-2014 (most recent data available), breast cancer mortality decreased by 38 percent, avoiding about 300,000 deaths. This decline in mortality is due to improved cancer treatment and early detection.”
Knowledge Is Power
In October, 1985, the American Cancer Society and the pharmaceutical division of Imperial Chemical Industries founded what is now referred to as National Breast Cancer Awareness Month (NBCAM). From the beginning, the goal of the NBCAM has been to educate and promote early detection through mammography as the most effective tool in the fight against breast cancer.
In 1980, a promise was made to a woman named Susan G. Komen by her sister Nancy Brinker. Nancy promised her dying sister that she would “do everything in her power to end breast cancer forever,” and in 1982, two years after Susan’s death at the age of 36, Nancy established the Susan G. Komen Breast Cancer Foundation. Since that time, the Susan G. Komen foundation is now the “largest nonprofit source of funding for the fight against breast cancer.” Their goal is to fund research, promote education and detection, and fulfill the promise made over 30 years ago.
Knowledge is power. Knowledge provides options and choices. Knowledge means that patients don’t have to settle because they simply don’t know any better. Power is trusting your intuition and fighting to be heard. Become knowledgeable about breast cancer. Learn the signs and symptoms and know that you are not alone.